“Well, the CT scan was negative, but we best do a lumbar puncture to make sure this isn’t a brain bleed”.
When people present to the Emergency Department with acute onset headache (typically described as worse headache of their life!) we need to think about a spontaneous intracranial hemorrhage. We need to be mindful (pardon the pun) of the causes of these non-traumatic bleeds with the most prominent cause being aneurysmal bleeding. This is an important distinction to make because patients with aneurysm may be amenable to an endovascular procedure to stop the bleeding or prevent a second bleed from occurring later in life. So in today’s article presentation we will look at a study which looks to answer the question – “how good are CT scans at detecting subarachnoid hemorrhage?
Title:
Sensitivity of modern multi-slice CT (MSCT) for subarachnoid hemorrhage at incremental timepoints after headache onset: a 10-year analysis. 1
Population:
Retrospective analysis of electronic records from Christchurch Hospital and included 347 patients who were diagnosed with atraumatic subarachnoid hemorrhage January 2008 & December 2017. They had important exclusion criteria:
- Cases miscoded as SAH
- Traumatic SAH
- Repat SAH admission
- SAH found on postmortem assessment without CT scan
- The day of onset of headache was not recorded
- Patient transferred to the investigation center without imaging or note access
- Patients with lost or destroyed records
The mean age was 59.9, with a greater percentage of women included (64.6%). The onset of headache was an important baseline characteristic, with the occipital being the most common location when identified. 62% of patients had GCS >14 with under 20% of patients having GCS 8 or less.
All patients had a MSCT, some had MSCT and lumbar puncture and patients either had CT angiography or MR angiography to assess for aneurysm.
Intervention:
Use of multi-slice CT scan (MSCT) for the detection of SAH in patients with acute atraumatic headache. The MSCT scanners are typically third generation machines (4th & 5th are also available but not widely used) which have increased capabilities including image noise reduction, increased resolution and reduced motion artefact. This is due to a combination of upgrades to the scanner itself as well as the software that drives the image generation.
Comparison:
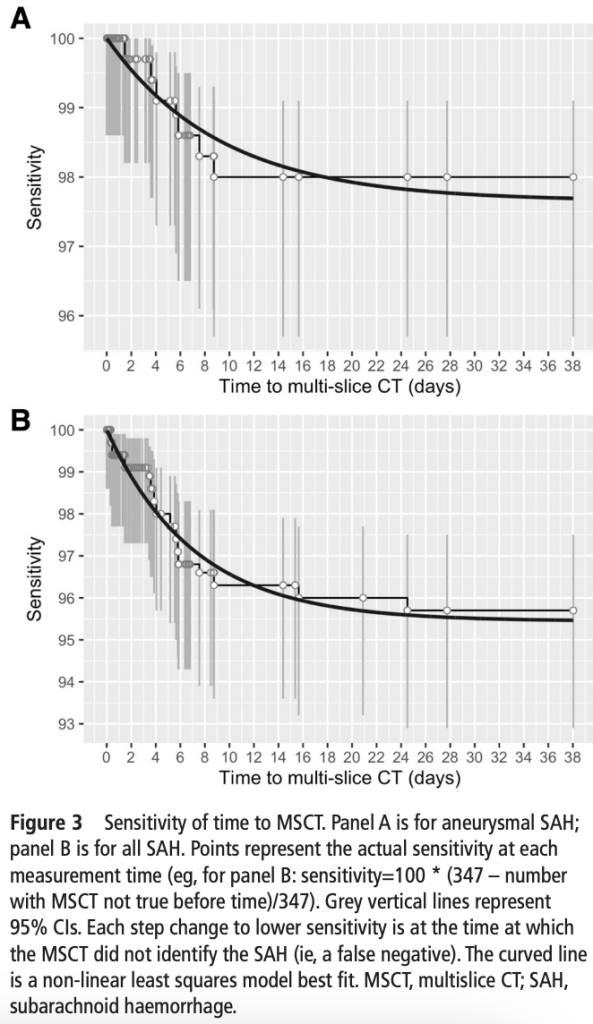
The researchers attempted to look at the sensitivity over time from onset of symptoms (in this case headache with structured estimates in patients who were missing this data).
They calculated sensitivity for multiple time windows (0-6, 0-12, 0-24, 0-72 & 0-96 hours)
Outcome:
Primary outcome
- The proportion of patients with spontaneous aneurysmal SAH that had a positive MSCT
Secondary outcome
- The proportions of patients with any spontaneous SAH that had a positive MSCT
Time to MSCT was defined as the duration from headache onset until the time the MSCT was performed.
Of the 347 patients with SAH, 260 were aneurysmal SAH – of note this paper included very few patients who had scans beyond 24 hours so the authors recommended caution in interpretation of the very high sensitivity found for time windows greater than 24 hours.
Sensitivity for aneurysmal SAH:
- 6 hours 100%
- 12 hours 100%
- 24 hours 100%
- 48 hours 99.6%
- 72 hours 99.6%
- 96 hours 98.7%
All SAH
- 6 hours 100%
- 12 hours 99.2%
- 24 hours 99.3%
- 48 hours 99.0%
- 72 hours 99.0%
- 96 hours 97.8%
30,000ft view:
The big picture here is that headaches are a very common presentation in the Emergency Department. Subarachnoid hemorrhage (SAH) as a cause for this is very rare, but when present – deadly with a breathtaking mortality rate (65% at one year) if untreated. 2 Remember what you were told in medical school about the presentation of SAH – “It’s the worst headache of my life, and it felt like I was kicked in the back of the head.” Or “I was having intercourse and got a terrible headache while having an orgasm.” It is important to remember that the presentation can be subtle with concerns associated with historical features, including syncope, vomiting, neck pain, and seizures. Focal neurological deficits may be present in only 50% of cases; the remainder will have a normal neurological examination.
This paper had very high sensitivity (>99%) through 24 hours, which is inconsistent with other published data. A meta-analysis by Dubosh et al. looking at aneurysmal SAH demonstrated a pooled sensitivity of 98.7% and specificity of 99.9% at 6 hours in a population with classic SAH symptoms (no focal neurological exam findings, no meningism). 3
What about a lumbar puncture (LP)? Perry et al. demonstrated that a cut of 2000 x 106 RBC in the fourth tube combined with no xanthochromia captured all patients with an SAH regardless of blood in the first tube. That should be good news to those who struggle to get “champagne taps”. 4

So, should we do CT angiography to find the culprit aneurysm? This is another excellent question, and to answer this, we need to know about the sensitivity of CTA when looking for an aneurysm. The good news is that the sensitivity of a negative non-contrast CT and CTA >6 hours from the onset of the headache is 99%. But CTA itself is 92.3% sensitive for aneurysms <4mm. 5
How should this modify your practice:
Overall, the pooled sensitivity reported by the authors is very high at 24 hours. This data is at odds with other data for the timeframes 6-24 hours. I would therefore recommend caution in interpreting this data for the 6-24 hour time windows.
Here is my diagnostic approach to headaches in light of this data. I asked the patient if they were worried they had bleeding in the brain and if they came here today for a CT scan of their brain. If they are adamant about wanting a CT scan, I will order a non-contrast CT brain – anecdotally, this will improve their anxiety, particularly if negative. In concert with this, I will give them my typical “migraine cocktail” (acetaminophen/paracetamol, ketorolac, prochlorperazine, lactated ringers +/- ondansetron).
For the 0-6 hour time window:
- CT non-contrast – if negative and their symptoms have improved, discharge home
- CT non-contrast – if negative and still symptomatic and never had a CTA before
- CTA head – if negative, then shared decision-making about LP but feel pretty good about sending them home
For patients presenting beyond 6 hours:
- CT non-contrast and CTA head – if negative, discuss adding an LP which if negative, feel very happy sending home
Marcolini have an excellent flow chart to describe their management process which I agree is very reasonable. 2
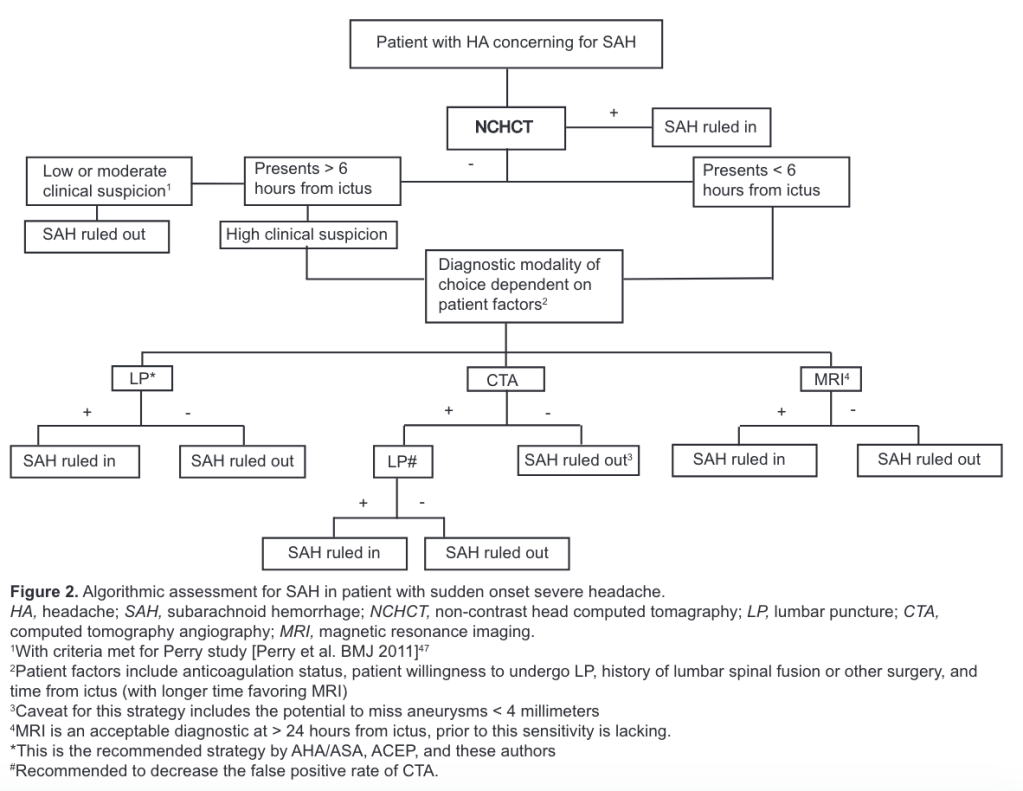
Shared decision making as always, is very important, particularly when it comes to making decisions about sending patients home.
Author: Dr Adrian Cois, MD
Assistant Professor
Emergency Medicine
@dr_cois
Extend Yourself:
- Read through the Marcolini review of management of SAH which is also the recommended approach from the American College of Emergency Physicians. 2
References:
1. Vincent A, Pearson S, Pickering JW, et al. Sensitivity of modern multislice CT for subarachnoid haemorrhage at incremental timepoints after headache onset: a 10-year analysis. Emerg Med J EMJ. 2022;39(11):810-817. doi:10.1136/emermed-2020-211068
2. Marcolini E, Hine J. Approach to the Diagnosis and Management of Subarachnoid Hemorrhage. West J Emerg Med. 2019;20(2):203-211. doi:10.5811/westjem.2019.1.37352
3. Dubosh NM, Bellolio MF, Rabinstein AA, Edlow JA. Sensitivity of Early Brain Computed Tomography to Exclude Aneurysmal Subarachnoid Hemorrhage. Stroke. 2016;47(3):750-755. doi:10.1161/STROKEAHA.115.011386
4. Perry JJ, Alyahya B, Sivilotti MLA, et al. Differentiation between traumatic tap and aneurysmal subarachnoid hemorrhage: prospective cohort study. The BMJ. 2015;350:h568. doi:10.1136/bmj.h568
5. Molyneux A. International Subarachnoid Aneurysm Trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised trial. The Lancet. 2002;360(9342):1267-1274. doi:10.1016/S0140-6736(02)11314-6

Leave a comment