This blog is going to be a little different. Here, I want to discuss two simultaneous papers to help better understand an approach to evaluating and managing renal colic. What is renal colic, I hear you say? Essentially, renal colic is a clinical entity where a person has a stone travelling from the kidney down through the ureter and down into the bladder. Most patients will experience SEVERE pain. The pain is colicky (coming and going in waves), sometimes associated with gross hematuria (blood you can see in your urine) and microscopic hematuria (blood in your urine that you can’t see). This happens when stones of various sizes go down the urinary tract, most commonly getting stuck at the ureterovesicular junction (where the ureter joins the bladder). A blockage anywhere along the tract can cause hydronephrosis (fluid accumulation in the kidney. As these spikey little stones make their way down the ureter, they rip up the inside of that pipe and cause pain as the ureter contracts against the blockage. It has been described as a painful experience as close for men to what labor contractions feel like for women. Having seen many women in labor and many men with renal colic, I’m going to sit on the fence and neither confirm nor deny the accuracy of this comparison.

Title:
Usefulness of protocolized point-of-care ultrasonography for patients with acute renal colic who visited Emergency Department: A Randomized Controlled Study. 1
Population:
Emergency Department patients with acute renal colic. Notably, they excluded patients with a recent diagnosis of stones within 30 days before arrival and those with fever >37.2C. Conducted at a single-center tertiary hospital with 78,000 monthly visits in Seoul, South Korea. Outcomes for 146 patients were analyzed, with 128 diagnosed with a stone.
Intervention:
Randomized controlled trial in which patients were assigned to either point of care ultrasound (UG) or conventional group (CG) on alternating days for five months.
Bedside US was performed by 12 attending Emergency Physicians or 14 resident Emergency Physicians who underwent a 4-hour education package and 10 cases of practice. The US looked at each kidney in short and long axis with the color Doppler mode applied to distinguish the renal collection system from the renal vessels.
Comparison:
The UG had a bedside point-of-care ultrasound performed to assess for hydronephrosis. Patients with hydronephrosis had a confirmatory CT performed. The CG group had a contrast or non-contrast CT scan. Both groups had an assessment of CBC, electrolytes, chemistry profiles, and urinalysis.
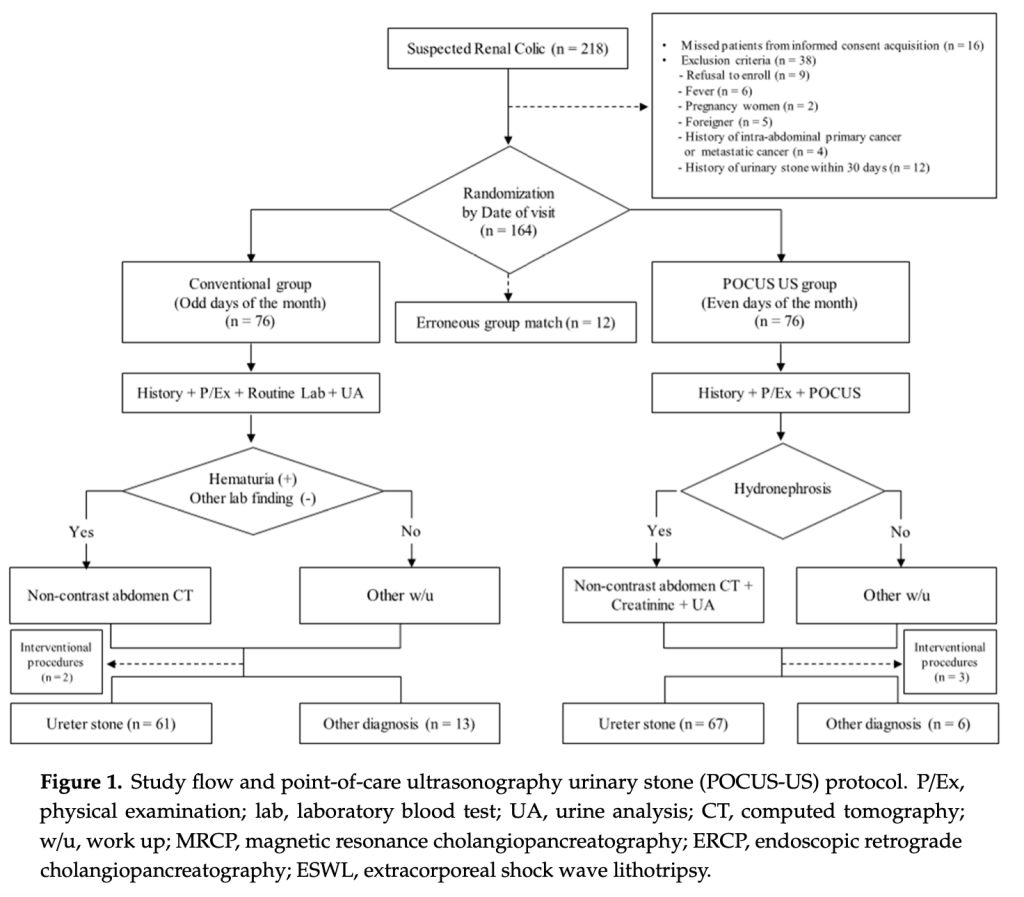
Outcome:
Primary outcome:
- ED length of stay – significantly lower in US group than conventional management group
- UG 172min (95% CI) [151-194min] versus CG 234min (95% CI) [216-252min]
- P-value <0.001
Secondary outcomes
- ED medical cost
- Significantly lower in UG than CG difference of $60 USD
- Incidence of acutely missed or delayed high-risk diagnoses.
- No significant difference
- Complications within 30 days
- No significant difference
Title:
Atomized intranasal ketorolac versus intravenous ketorolac for treatment of severe renal colic in the Emergency Department: A double-blind, randomized controlled trial. 2
Population:
Emergency Department adult patients with acute severe renal colic with a numeric pain scale >7.0 out of 10. A total 176 patients were randomized (5 withdrew as they rescinded their consent for participation) – 85 in the IN group and 86 in the IV group.
Intervention:
Double-blind randomized controlled trial with participants randomly assigned (1:1) to receive single doses of either intranasal (IN) or intravenous (IV) ketorolac.
Comparison:
30mg IV ketorolac compared with 30mg IN ketorolac (half in each nostril). They blinded this trial by giving 0.9% normal saline 1mL IN or 0.9% normal saline 10mL IV, respectively. Compared initial numerical pain scores “no pain at all” (0) and “worst pain ever” (10).
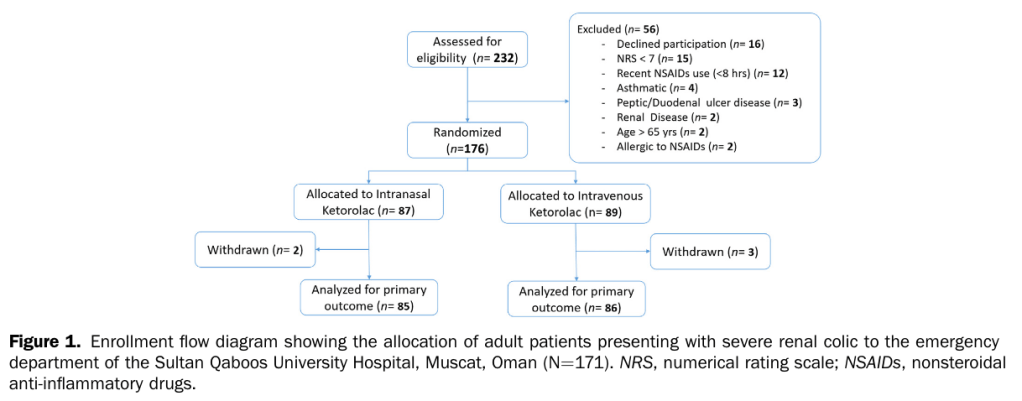
Outcome:
Primary outcome:
- Change in numeric pain score at 30 and 60 mins.
- The 30-min average difference in pain score was 0.69 (95% CI) -0.08 – 1.48
- The 60-min average difference in pain score was 0.10 (95% CI) -0.85 – 1.04
Secondary outcomes
- Treatment success at pain score <3.0 at 60 mins
- 69.8% of IV and 67.1% of IN
- Adverse events (e.g., nausea, vomiting, allergic reactions)
- No reports of significant adverse effects
- There was no difference in the need for rescue medications.
- 11.6% of IV and 10.6% of IN
- Revisits to the ED within 24 hours
- 18.6% of IV and 17.6% of IN
30,000ft view:
In a world with increasing pressure to speed up and get our patients their final disposition while minimizing risk, these two papers provide an interesting perspective on an approach providers can utilize. As with all POC ultrasound research, the degree of competence is mainly responsible for the reliability of the data. The sonographers in the study had a very comprehensive education package – something that could easily be achieved if learners focused on this during their training. There is no reason resident physicians can’t become competent in renal ultrasound by the time they complete their training. When a patient presents with symptoms suggestive of renal colic, these two papers seem to suggest that you could dip their urine (to make sure it’s not infected), perform a renal US (to assess for hydronephrosis), and give them 30mg of IN ketorolac. If they are symptomatically improved, you could have a shared decision-making conversation with them and discharge them for outpatient multimodal analgesia and primary follow-up. Following this approach, you would have achieved adequate pain relief by 60 minutes in around 70% of cases – no needles, no radiation from a CT scan. That’s pretty good if you ask me! The more challenging question would be, who do I need to scan with a CT? To my mind – folks who do not have adequate resolution of pain by 60 minutes, those with infection, or those with complicated renal history (prior complicated stones, renal transplant, or those who look sick). As always, more data is needed, and there are limitations for each of these studies. They were both single centers, with limits to the protocol’s generalizability and the skill of the sonographer being two of the most prominent factors.
How should this modify your practice:
This is always a tricky question to answer, given how small each trial is, and I encourage caution when making clinical practice decisions based on these data. However, there is a signal here indicating we could do things differently to decrease time in the department and reduce exposure to risk with CT radiation and intravenous use of analgesic medication. I try to perform a bedside US for patients who are experiencing renal colic – sometimes, I am not able to, owing to competing interests. However, in a world where we are increasingly seeing patients from the waiting room, I think that there is some merit in performing bedside US and giving intranasal medications for patients experiencing renal colic because if these data pan out – we could save time and limit exposure to risk for our patients.
Author: Dr Adrian Cois, MD
Assistant Professor
Emergency Medicine
@dr_cois
Extend Yourself:
I recommend you visit the Core Ultrasound website and view this video. This should also serve as a plug for this website in general. It is an amazing resource for novice and experienced sonographers alike. 3 https://coreultrasound.com/hydronephrosis/
References:
1. Kim SG, Jo IJ, Kim T, et al. Usefulness of Protocolized Point-of-Care Ultrasonography for Patients with Acute Renal Colic Who Visited Emergency Department: A Randomized Controlled Study. Medicina (Mex). 2019;55(11):717. doi:10.3390/medicina55110717
2. Al-Khalasi USS, Al-Alalawi AKSAS, Al-Jufaili M, et al. Atomized Intranasal Ketorolac Versus Intravenous Ketorolac for the Treatment of Severe Renal Colic in the Emergency Department: A Double-Blind, Randomized Controlled Trial. Ann Emerg Med. 2024;83(3):217-224. doi:10.1016/j.annemergmed.2023.10.009
3. read 5 Minute Sono··1 min. Hydronephrosis – Core Ultrasound. Published February 14, 2020. Accessed February 23, 2024. https://coreultrasound.com/hydronephrosis/

Leave a comment