I love this question. Mostly because I can lean on my favorite Emergency Medicine paper – the Salt-ED trial; this was a pragmatic, cluster randomized control trial – essentially a methodology that mimics real clinical situations where the researchers replaced all the fluid in the department with a certain crystalloid for a calendar month at a time over 16 months total.
So, let’s dive into the paper and figure out how we can answer the above question in an evidence-based manner!
Title:
Balanced crystalloids versus saline in noncritically ill adults. 1
Population:
13,347 patients received >500mL of crystalloid and were hospitalized outside an ICU. They were adults >18yo, with those who received <500mL being excluded due to a low dose of exposure to the intervention.
Intervention:
Emergency Departments were stocked with balanced crystalloids (plasma-lyte / lactated ringers) alternating with normal saline. Physicians had to use the fluid stocked for their patients for that month (they were blinded). They could choose a specific fluid if they felt it was clinically indicated for a particular patient.
Comparison:
The study sought to understand the difference between the administration of balanced crystalloid and normal saline on a composite of death/hospitalization, kidney failure, and renal replacement therapy. This was done at Vanderbilt University with a similar trial in critically ill patients with a similar study design. 2
Outcome:
The baseline characteristics of the two groups were similar which included demographics and presenting laboratory values. Of note only around 20% of patients were black or other non-white race.
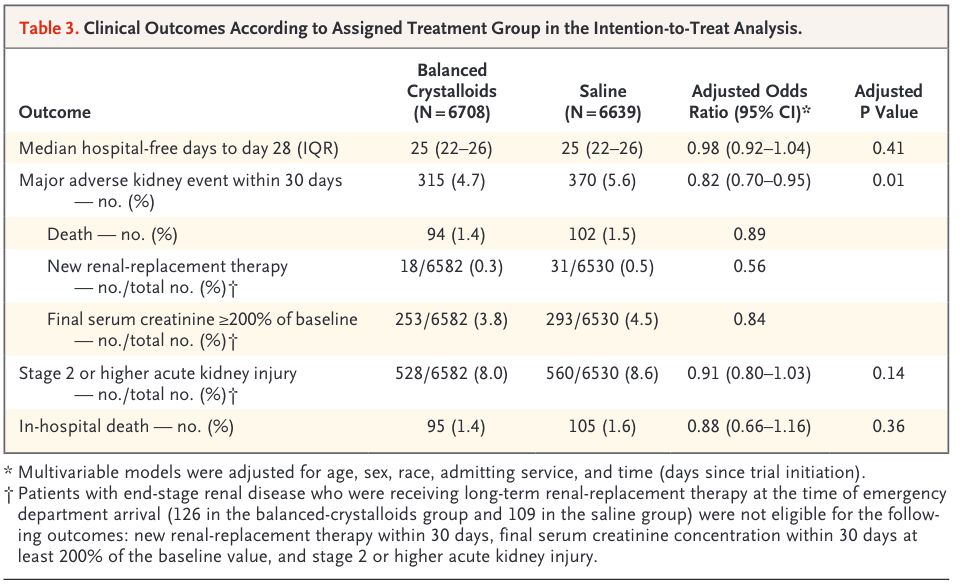
Primary outcome:
- Hospital-free days to day 28, a composite of in-hospital death and hospital length of stay
- No difference between groups
Secondary outcomes:
- Major adverse kidney events within 30 days (death, New RRT, final serum creatinine >200%)
- Adjusted odds ratio (95% CI) 0.82 (0.70-0.95) P=0.01
- Acute kidney injury of stage 2 or higher
- No statistically significant difference
- In hospital death
- No statistically significant difference
30,000ft view:
This is my favorite Emergency Medicine trial. It was genuinely practice-changing for me and profound because in medical school back in Australia, it was drilled into me to give Normal Saline for fluid resuscitation, and that was a mantra that I had stuck in my mind. Some crucial limitations or criticisms of the paper include that the population was predominantly white, so generalizability is not certain. I have seen others criticize the only statistically significant secondary outcome being a composite. I’ve seen it called signal boosting! But this is okay and appropriate, mainly because the other outcomes are essentially death! That would be a pretty drastic outcome for a simple change in the type of fluid administered, and I would suggest that we look for the more subtle physiologic changes associated with the kind of fluids we give.
How should this modify your practice:
I strongly recommend that the answer to my opening question is almost always lactated ringers, and if you end up giving normal saline – make it no more than 1000mL. The results of this study have also given rise to my favorite pharmacology-related joke – I don’t call it normal saline; I call it ABNORMAL saline. That is because it has a supraphysiologic chloride load and thus predisposes patients to develop hyperchloremic acidosis, which is the proposed mechanism behind the difference between the two groups in this trial. But what if they are also receiving our favorite antibiotic, ceftriaxone, which isn’t compatible with LR? Then put another line in for the antibiotic administration!

Author: Dr Adrian Cois, MD
Assistant Professor
Emergency Medicine
@dr_cois
Extend Yourself:
- Read the primary article here 1 – https://doi.org/10.1056/NEJMoa1711586
- Breakdown from “The Bottom Line” 3 – https://www.thebottomline.org.uk/summaries/icm/salt-em/
- Breakdown from “2 Minute Medicine” 4 – https://www.2minutemedicine.com/salt-ed-normal-saline-versus-balanced-crystalloids-in-noncriticaly-ill-adults/
References:
1. Self WH, Semler MW, Wanderer JP, et al. Balanced Crystalloids versus Saline in Noncritically Ill Adults. N Engl J Med. 2018;378(9):819-828. doi:10.1056/NEJMoa1711586
2. Semler MW, Self WH, Wanderer JP, et al. Balanced Crystalloids versus Saline in Critically Ill Adults. N Engl J Med. 2018;378(9):829-839. doi:10.1056/NEJMoa1711584
3. SALT-ED – The Bottom Line. Accessed February 6, 2024. https://www.thebottomline.org.uk/summaries/icm/salt-em/
4. SALT-ED: Normal Saline versus Balanced Crystalloids in Noncriticaly Ill Adults [Classics Series] | 2 Minute Medicine. Published June 22, 2022. Accessed February 6, 2024. https://www.2minutemedicine.com/salt-ed-normal-saline-versus-balanced-crystalloids-in-noncriticaly-ill-adults/

Leave a comment